Elevated levels of the Galectin-3 protein are associated with multiple disease processes, in addition to those Galectin Therapeutics is addressing in ongoing clinical trials such as fatty liver disease, psoriasis and cancer. Among those is disease of heart muscle and blood vessels.
Galectin Therapeutics is collaborating with a number of academic groups to evaluate cardiovascular diseases that might be amenable to treatment with our galectin inhibitor drugs. In this article, I discuss the results obtained by the outstanding investigators at the Vascular Biology Center and the Department of Pharmacology and Toxicology at Augusta University (formerly known as Georgia Regents University), which were recently presented at the 2016 American Thoracic Society International Conference and highlighted in a recent press article.
What is pulmonary arterial hypertension (PAH)?
Pulmonary hypertension (PH) is high blood pressure in the main arteries that supply blood to the lungs, caused by the narrowing and constriction of blood vessels in the lungs themselves. This elevated blood pressure increases the work required of the heart’s right ventricle to pump blood into the lung, which eventually culminates in failure of the right ventricle, circulatory collapse and death. The causes of PH have been categorized into five groups. Group 1, also called pulmonary arterial hypertension (PAH), includes idiopathic and hereditary PAH, as well as multiple disorders that affect the small arterioles (blood vessels) in the lung. The remaining four groups are secondary to other disease including left heart failure (Group 2), chronic lung disease (Group 3), chronic pulmonary embolism (Group 4) or multifactorial mechanisms (Group 5).
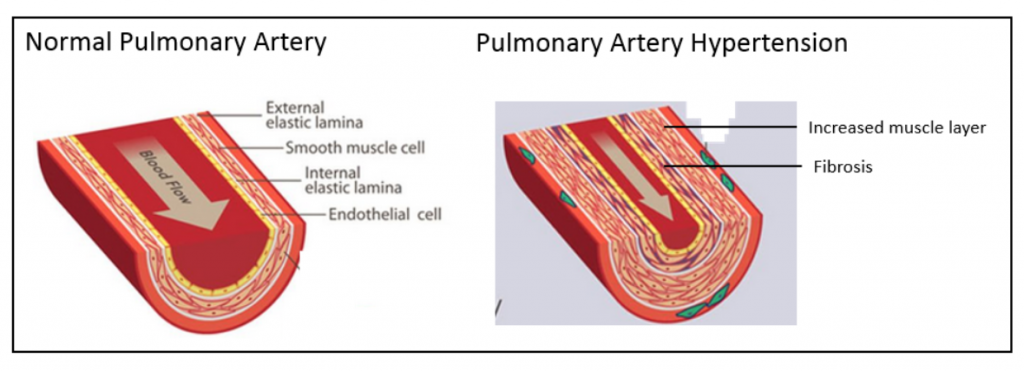
The figure below on the left shows a normal pulmonary artery with the various layers of cells in the wall, including the external elastic lamina on the outside of the artery, the smooth muscle cell layer, the internal elastic lamina and the endothelial cell lining on the inside. As depicted in the figure below on the right, in PAH there is a marked increase in the thickness of the smooth muscle cell layer as well as fibrosis. This narrows the lumen of the artery and restricts blood flow.
One of the more pressing needs is for new PH therapies in Group 1 disorders, particularly idiopathic PAH. Although there are a number of vasodilator drugs that are approved for the treatment of PAH, additional therapies are needed to address the structural narrowing of pulmonary arteries..
Galectin-3 protein is markedly elevated in human and experimental pulmonary arterial hypertension
The investigators at Augusta University experimented with three animal models of PAH using chemical treatments and/or low oxygen environments. These models are well established to cause narrowing of the pulmonary blood vessels leading to stress and failure of the right ventricle, meaning they mimic what happens in human PAH. The investigators found that the galectin-3 protein was markedly higher in the pulmonary arteries of diseased animals and the degree of increased blood pressure correlated with the level of galectin-3 elevation.
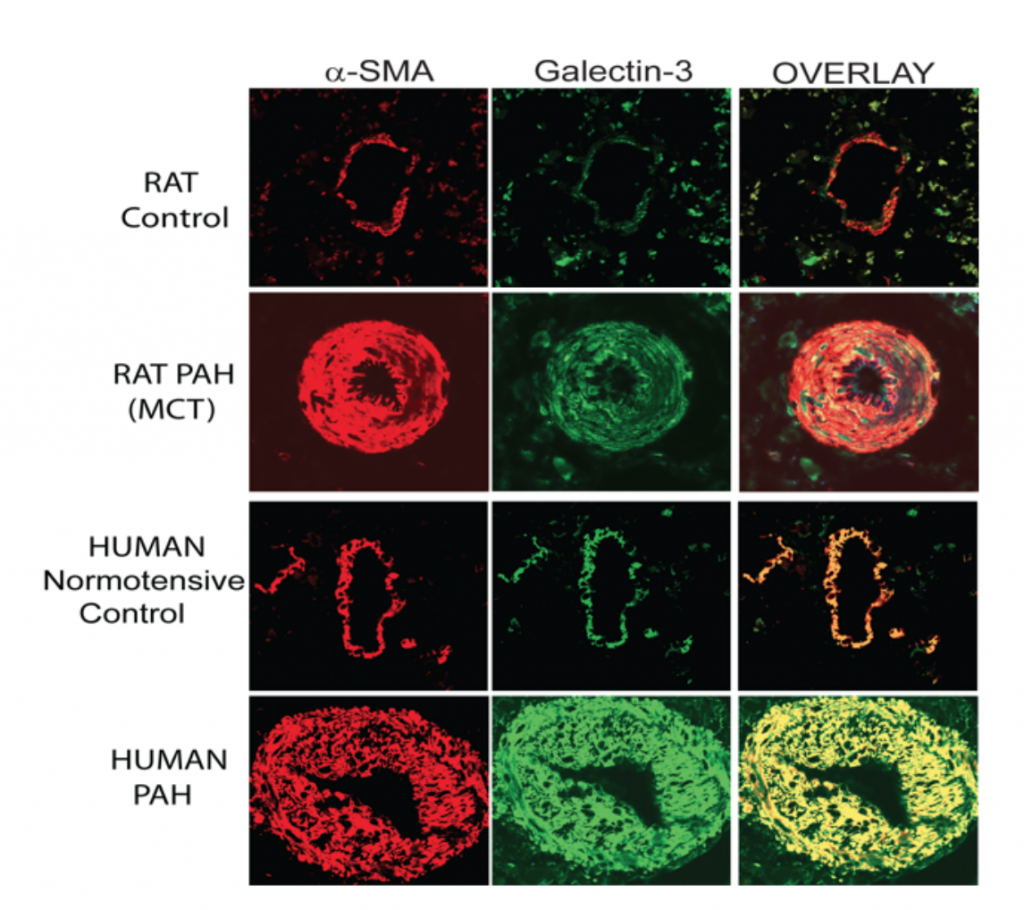
Since a picture is worth a thousand words, I have reproduced below images of the microscopic assessment of galectin-3 in pulmonary arteries in one rat model with monocrotaline treatment (MCT), as compared with the human disease.
The red stain is for the protein alpha smooth muscle actin (α-SMA), which stains smooth muscle cells in the artery, and the green stain is for the galectin-3 protein; the overlay combines the two images and shows that galectin-3 is predominantly in smooth muscle cells. In both the normal rat and the human pulmonary arteries, a thin layer of smooth muscle cells that contain galectin-3 is visible. In the rats and humans with PAH there is a marked increase in thickness of the muscle cells that surround the artery associated with a marked increase in galectin-3.
GR-MD-02 is effective in experimental pulmonary hypertension
The investigators next tested whether our galectin-3 inhibitors were able to change the course of experimental PAH using the model in which the rats were given a single injection of MCT to induce pulmonary hypertension. Two of our galectin inhibitors were used as treatments: GR-MD-02, which is currently in clinical trials for NASH, psoriasis, and cancer, and GM-CT-01.
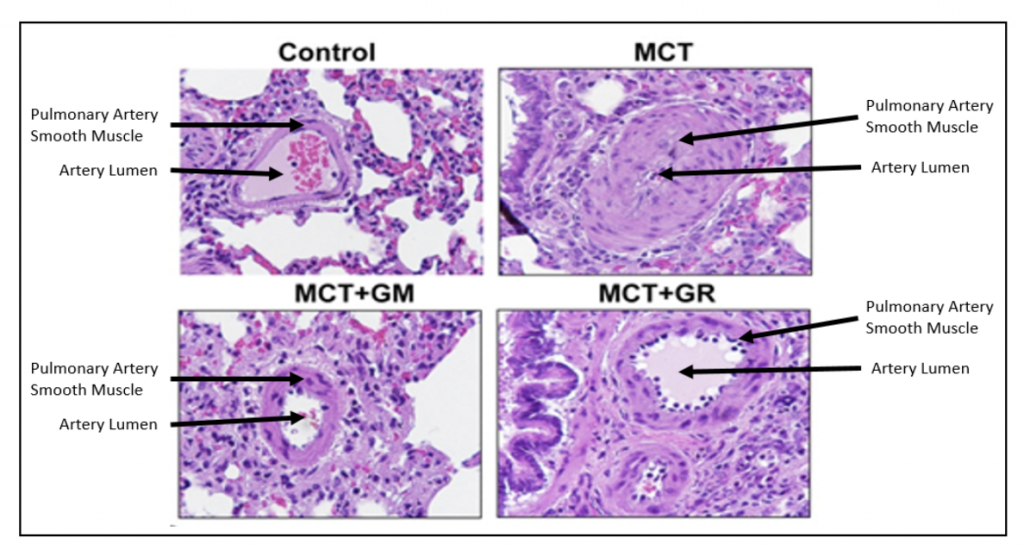
As shown in the figure below, the control (normal) rat pulmonary artery has a thin layer of smooth muscle cells surrounding it, whereas the animals treated with MCT have a markedly thickened smooth muscle layer that nearly blocks the lumen of the artery. Treatment of MCT animals with either GR-MD-02 or GM-CT-01 resulted in significantly fewer smooth muscle cells and a much larger artery lumen.
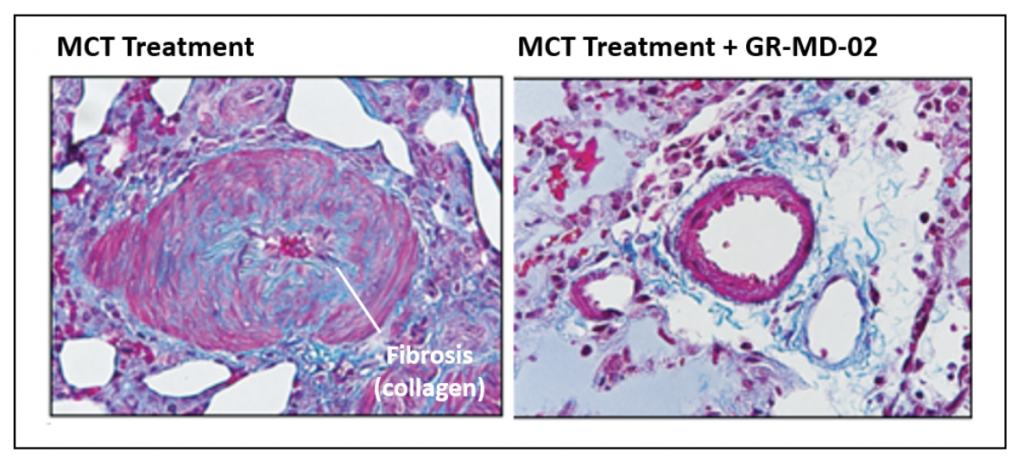
Below are images of pulmonary arteries stained to show fibrosis, mostly the protein collagen, which is identified by the light blue material. In the MCT treated animals, there is a significant amount of fibrosis associated with the smooth muscle cells in the pulmonary artery. This fibrosis is virtually eliminated in the artery wall following treatment with GR-MD-02, which provides a link to data showing improvement in fibrosis in other models of disease in liver, lung and kidney.
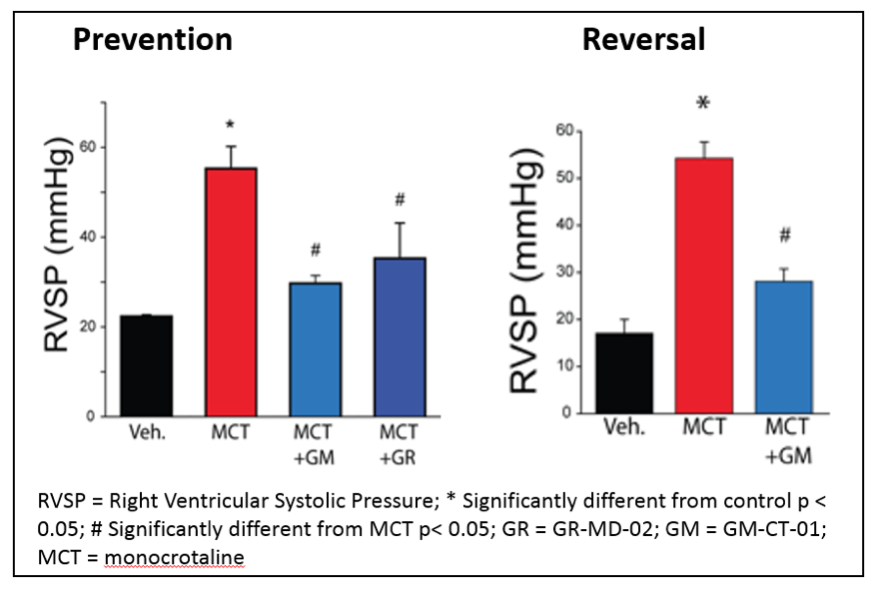
Treatment with either GR-MD-02 or GM-CT-01 also resulted in functional improvement in the PAH rats as indicated by reduced right ventricular systolic pressure (RVSP), as shown below. This improvement was seen whether the treatment was started immediately after the MCT injection (Prevention) or three weeks after the MCT injection (Reversal).
Prospects for human therapy
The results from these animal studies suggest that exploration of anti-galectin therapies, and specifically with GR-MD-02, might be a new therapeutic approach for these seriously ill patients. Currently there are approved therapies that help dilate constricted pulmonary arteries, but there are no therapies that effectively change the structure of the arteries or reverse the long-term course of the disease. A drug able to reverse the arterial smooth muscle and fibrosis findings in PAH might play an important role in treating these patients.
These “CEO Perspectives” are a regular feature of our communication activities and may contain forward looking statements within the meaning of the Private Securities Litigation Reform Act of 1995, including whether GR-MD-02 and GM-CT-01 may be effective in the treatment of pulmonary arterial hypertension. These statements relate to future events and use words such as “may,” “might,” “could,” “expect” and others. For a discussion of additional factors impacting Galectin’s business, see the Company’s Annual Report on Form 10-K for the year ended December 31, 2015, and subsequent filings with the SEC. You should not place undue reliance on forward-looking statements. Although subsequent events may cause its views to change, management disclaims any obligation to update forward-looking statements.






1 Comments found